India has now 10 reported cases of monkeypox and the country’s topmost biomedical research agency, Indian Council Medical Research (ICMR) has already started conducting analysis on the viral zoonotic disease and inviting pharmaceutical and diagnostic companies to bring out vaccines and testing kits. Following this, several health experts advised strengthening the surveillance to avoid silent transmission of Monkeypox.
According to the World Health Organization (WHO), over 38,000 cases of monkeypox have been reported across the world so far. Last month, the global health agency declared the monkeypox outbreak a global health emergency. It is noteworthy that at the moment the health agency uses this term for only two diseases: COVID-19 and Polio.
Nearly three years after the first case of COVID-19 was reported, with monkeypox the dangers of zoonotic diseases and the need for stringent research and surveillance links between human and animal health have again come under the spotlight.
What are zoonotic diseases?
Zoonotic diseases are a group of diseases caused by bacteria, viruses, or other parasites, that are passed on from animals to humans. Usually, the animals are not affected by the pathogen and are merely acting as a host. According to health experts, due to rise in the interaction between animals and humans, there is an increase in zoonotic diseases. According to WHO, 61 percent of all current human diseases are zoonotic in origin, and the report also adds that 75 percent of emerging human diseases are zoonotic. Moreover, health experts have warned that there are more and more diseases in the present world that are reaching epidemic or pandemic levels.
Zoonotic pathogens can spread to humans through direct contact or through food, water or the environment. According to public health experts, from Ebola to bird flu and Middle East Respiratory Syndrome (MERS) to Zika virus, the pathogens have encroached the world, as humans have encroached on wild spaces.
In the last two decades, emerging zoonotic diseases have been reported from 18 out of 22 countries in the region, often, with explosive outbreaks and high fatalities.
“Zoonotic disease emergence often occurs in stages, with an initial series of spillover events (spillover refers to the cross-species transmission of pathogens from wildlife to humans), followed by repeated small outbreaks in people, and then pathogen adaptation for human-to-human transmission,” Dr. Namita Jaggi, Chairperson- Lab services and Infection control & Chief- Education & Research, Artemis Hospitals told Financial Express.com.
Dr. Jaggi explained that HIV emerged from chimpanzees in Africa, spilling over to humans repeatedly before its global spread.
“We can take an example of HIV for better understanding. HIV emerged from chimpanzees in Africa, spilling over to humans repeatedly before its global spread.This initial phase of emergence was driven by bushmeat hunting and was the primary driver of its emergence. A second phase of emergence was driven by increased urbanization and road expansion in Central Africa beginning in the 1950s, and dispersal of index cases harboring prototype HIV-1 infections that were transmissible from person to person. The virus then entered the rapidly expanding global air travel network and became pandemic, with its emergence in North America, Europe, and Asia, accelerated by changes in sexual behavior, drug use, trade in blood derivatives, and population mobility,” Dr. Jaggi said.
‘The Animal-Human Spillover’
In recent months, multiple cases of various zoonotic diseases have been reported across the world and the latest in this list is Langya, reported in China, which is suspected to have come from shrewd.
“Human-animal Spill-over generally involves a “source host”: an animal responsible for shedding the pathogen; a “recipient host”: a human that is infected by the pathogen; and a “bridge/intermediate host”: a host species that acts as a bridge or link in the transfer of the pathogen between animal and human,” Dr. Jaggi explained.
Sometimes, the intermediate host can be a mosquito or bacteria. “The intermediate host may or may not be present in the spillover event. Exposure of the recipient host (human) to the new pathogen can occur either directly (e.g., through an animal bite or contact with contaminated secretion/blood) or indirectly (e.g., through a vector, or contact with contaminated feces or a surface containing the microorganism),” Dr. Jaggi told Financial Express.com.
According to Dr. Jaggi, the increased interfacing of human and animal is the main cause of these spill-over events.
“Handling, poaching, and consumption of meat from wild animals and derived products, selling of animals and their products in live animal markets for medicinal purposes or cultural practices, as souvenirs, pets, among other finalities. These markets contribute significantly to the interaction of humans with different species and new pathogens. In those places where different species are confined, pathogens can be transmitted not only through contact with meat, blood and other biofluids, but also through aerosols and contaminated surfaces,” She said.
Dr. Namita also pointed out that activities in sylvatic environments, such as deforestation and construction of human settlements in forest areas, also increase the interaction between humans and different species and for this reason are important drivers of spillover events.
Some recent Zoonotic disease outbreak around the world
The major outbreaks that have been linked to animals in recent years are:
Bovine tuberculosis: It was first identified in the late 19th to early 20th century, transmitted from cows to humans via bacteria present in milk of infected cows. It is passed between people via coughing or spit. Bovine TB remains endemic among cattle globally, there were nearly 143,000 bovine TB deaths in 2018.
Q Fever: Then there was an outbreak of Q fever in 2007 in the Netherlands, 50,000 people estimated to be infected. The Dutch government culled more than 50,000 dairy goats on 55 farms to control the spread of the disease. First identified in humans in the 1930s, Q fever was transferred from goat to humans via bacteria as an intermediate host.
Avian influenza or “bird flu”: It occurs naturally throughout the wild bird population, but until the 1990s few had suspected that it might transfer to humans. So when a three year-old boy died of respiratory failure in Hong Kong in 1997, it was initially thought to be viral pneumonia. A highly pathogenic strain of bird flu: H5N1 transmits via direct or indirect contact with infected live or dead poultry or contaminated environments, such as live bird markets. Infected birds shed avian influenza virus in their saliva, mucous and faeces. The disease is now endemic in poultry populations in Bangladesh, China, Egypt, India, Indonesia, and Vietnam. H5N1 continues to infect and kill hundreds of people, with more than 800 reported cases and 400 deaths between 2003 and 2019.
Nipah Virus: The first case of Nipah virus was detected in 1999 in Malaysia. The disease had transferred from bats to pigs, in which it was only a mild disease. But from infected pigs it was then a relatively easy jump to the humans that tended them. In humans the disease can cause acute respiratory infection and fatal encephalitis, and has an estimated case fatality rate of 40–75%. The initial outbreak saw 105 deaths, and led to the culling of almost 1 million animals. The subsequent outbreaks were found in India and Bangladesh.
Severe acute respiratory syndrome (SARS): The first case of coronavirus jumping from animal to humans was detected in 2002 in China when SARS outbreak occurred. Virus was traced back to horseshoe bats, who passed the virus on to masked palm civets before being transmitted to humans. There were only about 8,500 cases before the epidemic was stamped out; with a fatality rate of 10–11% over 800 people died. Thousands of farmed civets were culled. The epidemic was declared contained by July 2003.
H7N7 – bird flu: It is another example of a highly pathogenic avian influenza virus jumping to humans. First detected in humans in 2003, virus transmitted to human directly or indirectly after coming in contact with infected live or dead poultry. s many as 2,000 people may have been infected, with human-to-human transmission happening on a much larger scale. In the Netherlands alone the outbreak spread to more than 250 poultry farms and led to a quarter of the country’s poultry flock (30 million birds) being culled.
H1N1 swine flu: WHO declared the swine flu as a pandemic in June 2009. Earlier strains of the H1N1 virus passed from animals to humans through close contact with infected meat, such as at slaughterhouses. Later on the virus started human to human transmission via airborne spread and through infected droplets from a cough or sneeze. The estimated number of global deaths occured between 151,700 and 575,000 people, majorily in south-east Asia and Africa.
MERS- CoV: Middle East Respiratory Syndrome Coronavirus, first detected in humans in 2012 in Saudi Arabia, is a virus transferred to humans from infected dromedary camels. MERS-CoV has been identified in dromedaries in several countries in the Middle East, Africa and South Asia. In total, 27 countries have reported cases since 2012, leading to 858 known deaths due to the infection and related complications. MERS has a case fatality rate of 35%
SARS-CoV-2: The ongoing pandemic due to the outbreak of SARS-CoV-2 in China in 2019 has affected the whole world and led to over 6 million deaths globally. The source of the outbreak is still unknown but theories come around two competing ideas – Laboratory escape scenario or zoonotic emergence.
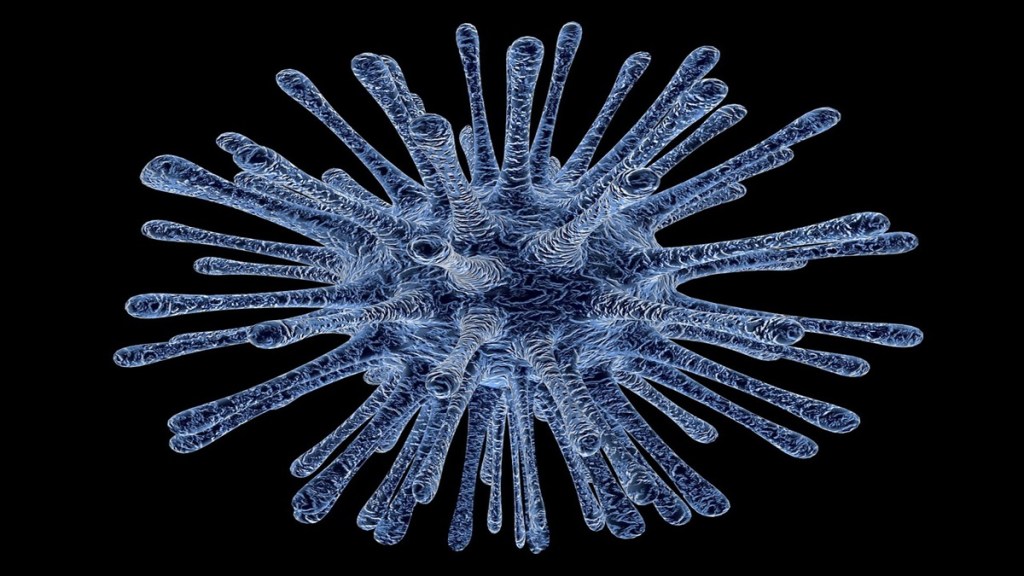
Monkeypox: Monkeypox virus is an enveloped double-stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family. There are two distinct genetic clades of the monkeypox virus: the central African (Congo Basin) clade and the west African clade. According to WHO, various animal species have been identified as susceptible to monkeypox virus. This includes rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates and other species. However, the natural history of monkeypox virus is still an uncertainity and further studies are needed to identify the exact reservoir(s) and how virus circulation is maintained in nature, according to WHO.
ALSO READ | China reports cases of Langya virus. What is this new zoonotic disease that has infected over 30 people?
Zoonotic diseases in India
In India, the major public health zoonotic diseases are rabies, brucellosis, toxoplasmosis, cysticercosis, echinococcosis, Japanese Encephalitis (JE), plague, leptospirosis, Scrub typhus, nipah, trypanosomiasis, Kyasanur forest disease (KFD), and Crimean-Congo hemorrhagic fever. Central Bureau of Health Intelligence (CBHI), India provisionally reported around 110 cases of rabies, 1674 cases of JE, 14971 cases of H1N1, 57813 cases of chikungunya, 4380 cases of kala-azar and 101,192 cases of dengue during 2018. Plague which has killed 12 million Indians keeps resurfacing regularly in different parts of India.
About 1.8 million receive anti-rabies vaccine, and 20,000 die of rabies every year. Brucellosis alone has contributed to loss of 30 million man days and economic loss of Rs. 24 crores a year. Japanese Encephalitis is endemic in many districts in Bihar and Uttar Pradesh. India reports 70% of global 58,200 kala azar cases.
ALSO READ | India may become a hotspot of zoonotic diseases, study reveals
In India according to an International Livestock Research Institute study, 13 zoonoses are the cause of 2.4 billion cases of human disease and 2.2 million deaths per year. The highest zoonotic diseases burden with wide spread diseases are in Ethiopia, Nigeria, Tanzania, and India.
According to experts, the increasing annual burden of Zoonoses on public health in India can be prevented only by effective periodic surveillance, pre-assessment or forecasting of zoonotic diseases and capacity building.
What are the economical impacts of zoonotic diseases?
Zoonoses have myriad impacts on human and animal health. According to global public health experts, the impact of zoonoses is hard to quantify – both human livelihood and well-being are severely affected.
A United Nations Environment Programme (UNEP) report has revealed that in the last two decades, emerging diseases have cost the world more than $100 billion. Experts have warned that if each of them turned into a pandemic, the loss would amount to trillions of dollars with every single infection.
According to Dr. Jaggi, the economy is also tremendously affected due to measures required for zoonoses control and eradication such as zoonoses surveillance, diagnosis, isolation and quarantine, restriction on animal transportation, treatment and vaccination programs, inspection of meat and milk, and biosecurity.
“From 1995 to 2008, the global economic impact of zoonotic outbreaks has exceeded 120 billion USD. If we look at the trends in recent years, SARS outbreak has impacted multiple sectors including the tourism sectors. The economic impact of SARS in Singapore, China, Hong Kong, and Taiwan was severe. Moreover, the emergence of the highly pathogenic avian influenza significantly curtailed tourism to Mexico and resulted in economic losses to the country. Likewise, India faced economic losses of around 900 crores due to the restriction of tourism and trades that resulted from the plague outbreak in 1994,” she said.
Dr. Namita Jaggi also highlighted that countries in the European Union were not spared from drastic economic losses resulting from the closure of export markets of poultry during the outbreak of highly pathogenic avian influenza.
“BSE is one of the important emerging zoonoses. The outbreak of BSE in Toronto, Canada, resulted in the loss of 0.5% of the city’s GDP. The disease was detected in millions of animals for which many countries banned international trade with Canada. The recent COVID-19 outbreak has significantly impacted the global economy. COVID-19 has significantly impacted all sectors of the society including health and education sectors, financial sectors, travel and hospitality sectors, and the sports sector. Travel industry is poised to lose significant revenue due to the pandemic,” she added.
It is estimated that millions of people will face extreme poverty due to the stalled growth resulting from this pandemic.
“We have seen what COVID-19 has done to the economic status of the world. It’s not just about the zoonotic diseases that cause an economic impact, it’s about the ability of the disease to cause a pandemic. As soon as it affects millions of people across, undoubtedly, it will cause a global economic impact. Over the recent years, as we have seen in COVID-19, there was significant economic burden all across the world, with loss of over trillions of dollars in the curbing of the pandemic as well,” Dr. Umang Agrawal, Infectious Disease Consultant, PD Hinduja Hospital & Medical Research Center, Mahim told Financial Express.com.
Current strategies for controling and managing zoonotic diseases
According to Dr. Jaggi, the control strategies for zoonotic diseases differ for each pathogen.
“Several practices are recognised as effective in reducing risk at the community and personal levels. Safe and appropriate guidelines for animal care in the agricultural sector help to reduce the potential for foodborne zoonotic disease outbreaks through foods such as meat, eggs, dairy or even some vegetables. Standards for clean drinking water and waste removal, as well as protections for surface water in the natural environment, are also important and effective. Education campaigns to promote handwashing after contact with animals and other behavioural adjustments can reduce community spread of zoonotic diseases when they occur,” she said.
Moreover, the global health agency is working with national governments, academia, non-governmental and philanthropic organizations, and regional and international partners to prevent and manage zoonotic threats and their public health, social and economic impacts.
Additionally, the WHO is also working to develop capacity and promote practical, evidence-based and cost-effective tools and mechanisms for zoonoses prevention, surveillance and detection through reporting, epidemiological and laboratory investigation, risk assessment and control, and assisting countries in their implementation.
“But making the policy is not enough, we have to overcome the challenges that exist in implementing the policy. There is an inadequate transparency regarding timely reporting of emerging zoonotic infections to WHO or any other international agency that is mandated to investigate and respond. Often medical authorities in the countries deny the existence of human cases, making it difficult for these agencies to understand the disease progression, Current SARS-CoV-2 pandemic could have been controlled if cases were reported on time,” she added.
Another challenge is the lack of effective collaboration between the animal and human health sectors under the concept of “One Health” approach.
Dr. Jaggi revealed that the detection and diagnosis of the disease has been considerably delayed due to difficulties in deploying teams for field investigation, lack of appropriate and safe sample shipment mechanism, lack of appropriate laboratory diagnostic facilities on-site or in-country, and insufficient capacities of the countries to plan, mobilize and implement appropriate control measures.
“There is also a lack of effective community participation and health education on zoonotic diseases. Overall, current strategies can prevent the next zoonosis outbreak, if implemented not only on paper but at regional, national and International level with the contribution of all the stakeholders,” she added.
‘Zoonotic diseases require effective control measures’
Zoonosis involves the interaction of humans, animals, and environment, and therefore a multi-sectorial approach is required to ensure effective control measures. According to Dr. Jaggi, the most important and critical technical areas that will need to be considered will include the following strategic approaches:
- Building effective collaboration between animal and human health sectors
- Improving surveillance for early detection of disease threats in humans
- Strengthening laboratory diagnostic capacities for novel pathogens
- Training of health-care workers on case management and infection control measures as well as pre-positioning of strategic supplies (investigation kits, personal protective equipment, etc.)
- Reducing transmission through social and behavioural interventions
- Developing epidemic preparedness and response capacities for emerging zoonoses – The plan should consider developing a geographic map of the distribution of zoonoses occurring in the countries using geographic information systems and other information technologies, and conducting a detailed risk assessment.
- Finally, there will be need to develop appropriate monitoring and evaluation tools and indicators to measure the progress of implementation of the strategic framework over time
According to health experts, the other challenges to the prevention and control of zoonotic diseases include weak surveillance and reporting systems and limited capacity for laboratory diagnosis of emerging zoonotic diseases such as SARS, Ebola, Marburg, and new strains of influenza.
ALSO READ | Climate change to increase the risk of emerging zoonotic infectious diseases: Study
‘The One-Health Approach’
One Health is an approach that recognizes that the health of people is closely connected to the health of animals and our shared environment. According to Dr. Jaggi, One Health is not new, but it has become more important in recent years.
“This is because many factors have changed interactions between people, animals, plants, and our environment – human populations are growing and expanding into new geographic areas, the earth has experienced changes in climate and land use, such as deforestation and intensive farming practices, the movement of people, animals, and animal products has increased from international travel and trade,” She added.
According to health experts, One Health is directly linked to the prevention and control of zoonoses. “This approach involves the participation of experts in human, animal, environmental health, and other relevant disciplines and sectors in monitoring and controlling public health threats and to learn about how diseases spread among people, animals, plants, and the environment,” she added.
The One Health approach can:
Prevent outbreaks of zoonotic disease in animals and people.
Improve food safety and security.
Reduce antibiotic-resistant infections and improve human and animal health.
Protect global health security.
By promoting collaboration across all sectors, a One Health approach can achieve the best health outcomes for people, animals, and plants in a shared environment, Dr. Jaggi pointed out.