In August, over 650 private hospitals in Haryana announced their exit from Ayushman Bharat, the Centre’s ambitious public healthcare scheme, reportedly over unpaid dues amounting to about Rs 490 crore. Not just Haryana, hospitals across India participating in the scheme have reported mounting financial strain due to delayed reimbursements from the government arising out of treating Ayushman Bharat patients. As per an estimate by the Indian Medical Association (IMA), unpaid claims amounting to over Rs 1 lakh crore are pending across public and private medical facilities.
Moreover, several hospitals across the country are awaiting empanelment from the Union health ministry to become part of the Ayushman Bharat network, a waiting even running into months. Healthcare institutions rue that the programme’s official package rates are unrealistically low, leading to a gap between the government’s claims of widespread reach and ground reality. Where private participation has declined over financial pressures, the burden has shifted to public hospitals—many already stretched thin.
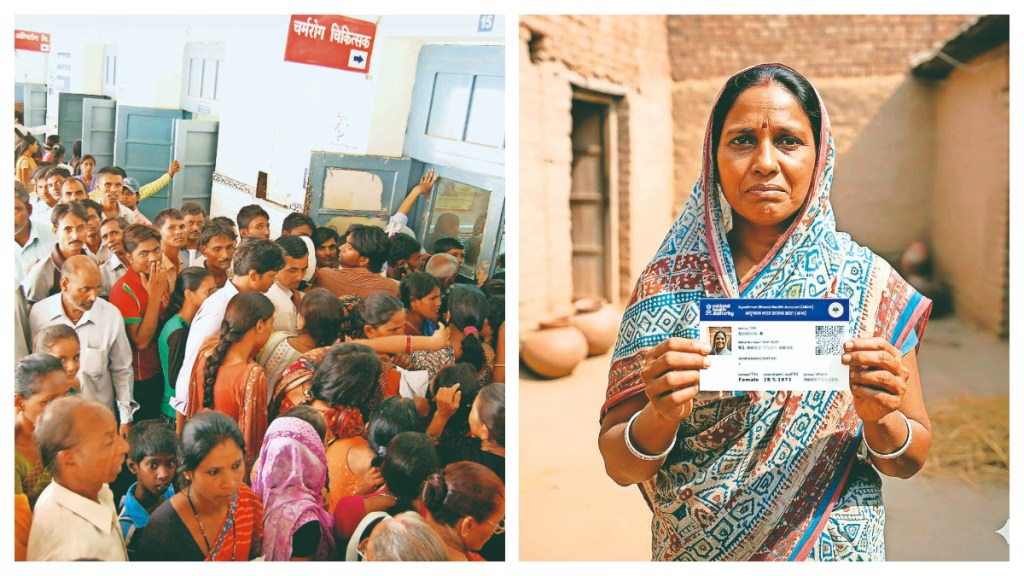
All this at a time when there is uneven public awareness. Even though the scheme is meant to benefit those in the low-income groups, awareness and the nearest empanelled facility are far out of reach.
Touted as the world’s largest publicly funded health assurance programme, the Ayushman Bharat—Pradhan Mantri Jan Arogya Yojana (PM-JAY) sought to bridge a long-standing gap between India’s rich and poor in access to quality medical care. When unveiled in 2018, it was heralded as a transformative leap towards universal healthcare. Seven years later, the initiative seems to be facing a few hiccups.
So, what’s ailing the Centre’s flagship mega health insurance scheme, also colloquially referred to as Modicare?
Scheme of things
Launched on September 23, 2018, the Ayushman Bharat PM-JAY has emerged as the world’s largest public healthcare scheme providing affordable medical care to millions of vulnerable households. As per the latest annual report of the National Health Authority (NHA), over 91.9 million hospital admissions have been facilitated under the scheme since its inception.
As of October 28 this year, over 420 million Ayushman cards have been issued, while more than 8.6 million senior citizens have been enrolled. According to reports, the scheme has saved beneficiaries more than `1.52 lakh crore in out-of-pocket healthcare costs since its launch.
Over 30,000 hospitals—55% public and 45% private—are empanelled under Ayushman Bharat PM-JAY. The scheme covers over 146.9 million families across India, providing them access to free treatment and quality healthcare.
As per reports, the scheme has had several positive impacts. According to a report published by The Lancet last year, there was a 36% increase in early detection and treatment of cancer over six years, attributed to Ayushman Bharat. Timely treatment, defined as starting within 30 days of diagnosis, improved significantly for the beneficiaries, who experienced a 90% increase in access compared to a 30% improvement for non-enrollees.
State of affairs
As per the NHA’s latest annual report released in October, the Ayushman Bharat scheme has 30,000 empanelled hospitals. “However, each state operates with a different rulebook,” IMA President Dilip Bhanushali explains.
In the national capital, where the scheme was launched in April this year, while nearly half a million Ayushman Bharat cards were issued, till September only about a few thousand surgical procedures have been recorded. According to the PM-JAY beneficiaries portal, Delhi has 178 empanelled hospitals so far, of which 46 are government hospitals and 128 private, with a reported health coverage of Rs 10 lakh for those aged over 70 years.
However, a further search shows a list of only 46 hospitals with the district-wise lists entirely lacking. And even so, of the informal lists that have been aggregated by medical organisations, several of the private hospitals named in the list are awaiting empanelment.
Those participating are reporting mounting financial strain due to delayed reimbursements across India. While the government’s guidelines promise settlement within 15 days of submission, “it is sadly true that Ayushman Bharat reimbursements sometimes take 6-8 months to get cleared”, as per Dr Bhanushali.
“As per the scheme, hospitals are meant to initiate the claim within 24 hours of the beneficiary patient’s treatment completion and discharge. But many hospitals will delay it or wait till the end of the week or month to submit all claims together, and not on a daily basis,” says Dr Vineeta Mittal of the IMA (UP chapter). Even when hospitals do often initiate the reimbursement claims on time, processing and approval from the state and the Centre cause delay.
Private hospitals, expected to be central to the scheme’s success, are among the hardest hit. In the recent and most popular case of Haryana, more than 650 hospitals threatened to withdraw services earlier this year, citing unpaid dues worth around Rs 490 crore. Other states, including Rajasthan, Manipur, Jammu and Kashmir, are also facing similar problems but at smaller scales, as per Dr Bhanushali of IMA, although he says they have not officially received any complaints.
Dr RV Asokan, former general secretary of the IMA, says such issues reflect a deeper policy neglect, highlighting how administrative lapses and underfunding or the lack of claim settlements threaten the scheme’s existence.
With Delhi and Odisha being the latest to join the scheme, the only state that remains is West Bengal, as per the NHA.
There also exists a difference in how Ayushman Bharat operates across the country. States such as Tamil Nadu, Uttar Pradesh, and Assam have fully embraced the scheme, integrating it with their own insurance models. Others like West Bengal have resisted, citing duplication of efforts of the existing state government. Prime Minister Narendra Modi has also openly criticised such states of neglecting public welfare in the name of politics.
And even among the included states, coverage of different treatments and procedures is not uniform since the state government decides which treatments to include. In Delhi, for instance, less than 150 diseases and procedures are covered, as per the NHA records. To add to this burden, new hospitals that have applied to be a part of the scheme are still awaiting empanelment. Delhi’s Sanjeevan Medical Centre, for example, is listed but is still waiting for official approval from the state, a spokesperson for the hospital shares. Similar is the case with Sri Balaji Action Medical Institute in the national capital.
Cost of healthcare
In addition to payment delays, hospitals argue that the programme’s official package rates are unrealistically low. Each medical procedure under Ayushman Bharat is assigned a fixed reimbursement amount, intended to standardise costs. However, these rates have not been revised meaningfully since 2018, even as inflation and medical expenses have risen, say experts.
Dr KK Singh, spokesperson for King George’s Medical University in Lucknow, says: “Given that we are a government hospital, nearly all of our facilities are already subsidised. However, it is true that medical expenses have risen while the package prices under Ayushman Bharat have not been revised accordingly.”
This becomes an issue for hospitals that depend mainly on private funding, and, therefore, have to be reimbursed for their spendings done on behalf of the government. “This becomes a real problem,” adds Dr Singh. For instance, a coronary bypass surgery that typically costs Rs 1.8 lakh in a mid-range private facility is reimbursed for less than Rs 1 lakh. Orthopaedic, oncology, and intensive care treatments show similar gaps. In the case of a hip replacement surgery, the Ayushman Bharat scheme covers the cost of only the surgery, but not the implant, which happens to be double the cost.
As per Dr Bhanushali, the IMA has repeatedly urged the National Health Authority (NHA) to revise rates periodically to reflect real costs. “We have approached and spoken to the NHA regarding revision of package rates, but no revisions have been made as of yet. The rates do not make sense as they currently stand—it is impractical.”
At the NHA review meeting held in Bhopal in October this year, announcements regarding the scheme’s success, hospital admission and claim investigations were made. “To accelerate progress, leadership of state and UT health authorities in digital integration and innovation will be key to making it the world’s largest transformative health scheme,” says Dr Sunil Kumar Barnwal, CEO of the NHA, suggesting that the state machineries for the scheme will need to be improved and enhanced for it to yield even better results. No mention was made or explanation offered on the failings of the scheme such as retreating private hospitals, delayed reimbursements, or even the stalled empanelments of hospitals.
Overflowing hospitals
As per the IMA, private healthcare facilities deliver almost 60% of inpatient care in India. This makes them an important tool for the programme’s reach. Yet, as financial pressures mount, several have scaled back involvement or pulled out entirely.
Where private participation has declined, the burden has shifted to public hospitals—many already stretched thin. Patients at government facilities frequently face long queues, overcrowded wards, and limited access to specialist care. In UP for example, despite being one of the states with the widest reach of the scheme, public hospitals find themselves overrun with patients and nearly always with a shortage of beds, forcing patients to seek private healthcare.
Dr Sanjay Kumar Verma, spokesperson for Lari Cardiology Centre in Lucknow, shares, “We have to refer at least seven to ten patients to other public or private hospitals each day.” The hospital, which now has a capacity of 100 beds, often refers patients not requiring emergency trauma care to other hospitals. At the government trauma centre in the same city, nearly 50 have to be turned away daily after administering emergency care, so as to manage a daily intake of approximately 130 patients with their 460-bed capacity.
Dr Verma says, “Both the patients as well as doctors referring to them hope that they can continue treatment at another public hospital, since the patients coming to us aren’t very financially stable,” he says. “But the rush at almost every government hospital in the capital of UP is so high, particularly at night, that we are left with no option.” A fleet of ambulances are always at the ready, not just to bring patients to the hospital, but to attempt to transfer them to other hospitals when the need arises.
Dr KK Singh of KGMU adds: “Our patient load is enormous. When we run out of beds, we are forced to provide emergent care and refer the patient ahead to a different government hospital or private hospital (which most serious patients can already hardly afford), for them to be admitted and treated further.”
Last-mile connectivity
Since Ayushman Bharat relies on digital infrastructure to manage claims, empanelment, and beneficiary identification, many doctors, especially in government hospitals, attest the system is cumbersome for those without access to technology and the digital know-how. In rural areas, unreliable internet connectivity and a shortage of trained administrative staff make compliance with things like diagnostic reports, discharge summaries, and patient documents difficult, they say.
Nationwide standardisation of the scheme remains elusive. The PM-JAY national dashboard itself is faulty, and has remained stuck on the same numbers for weeks, even as empanelments and withdrawals continue. The other prong of this issue is that of uneven public awareness. Many eligible families either do not have their health cards or are unaware of how to use them or acquire them.
Sanjeev Paswan, 47, a native of Bihar working at a Delhi Metro construction site, recently visited AIIMS in the national capital after he fainted due to low blood pressure and dehydration. An Ayushman Bharat card-holder in his native state, Paswan was unaware that Delhi had become a part of the network now.
“If I knew, I would have used it. Thankfully I was only admitted for a few hours at night for observation,” he shares, saying that if his condition was more serious, without the Ayushman Bharat card or the government subsidies offered by AIIMS, he might have found himself in a rather difficult situation.
Policy analysts and hospital associations have been proposing suggestions for bettering the scheme’s functioning and inspiring renewed confidence. “These measures include ensuring of time-bound reimbursements for hospitals, revision of package rates based on current costs, better fraud detection tools, better centre-state coordination, simplified empanelment as well as grievance redressal systems, and further investment in public healthcare,” lists Dr Bhanushali of the IMA. “More than 1.9% of the GDP has to be spent on healthcare for these issues to be resolved,” he adds, referring to the government health expenditure of 2023-24.
In an interview, Abhimanyu Saxena, head of health system strengthening at the United Nations Development Programme (India), had said that India’s model can still set a precedent globally if managed well. “Not just Asia, but the world can also adopt Ayushman Bharat because it demonstrates how public insurance can reach large populations if systems are transparent and accountable,” he was quoted as saying in reports.
In Numbers
- 450 million Ayushman Bharat beneficiaries across India
- 30,000 hospitals empanelled under the scheme
- 91.9 million hospital admissions facilitated under the initiative
- 96% grievance resolution rate achieved by the mission
- 15.7 million ABHA App downloaded so far
- 404.5 million Ayushman Bharat cards issued
Glaring Gaps
- Slow adoption across states; West Bengal still not part of scheme
- Non-uniform coverage provisions; Delhi provides Rs 10 lakh, while other states Rs 5 lakh
- Lack of awareness among rural populations, low-income groups
- PM-JAY portal prone to crashes, poor updation of hospital details on dashboard
- Beneficiaries unaware of empanelments, corresponding eligibility; delays, discouragement in seeking treatment
- Settlements can take weeks to months due to tedious clearance, reimbursement process
- Package rates not uniformly revised with current costs and inflation, resulting in out-of-pocket expenditure and labour for private hospitals