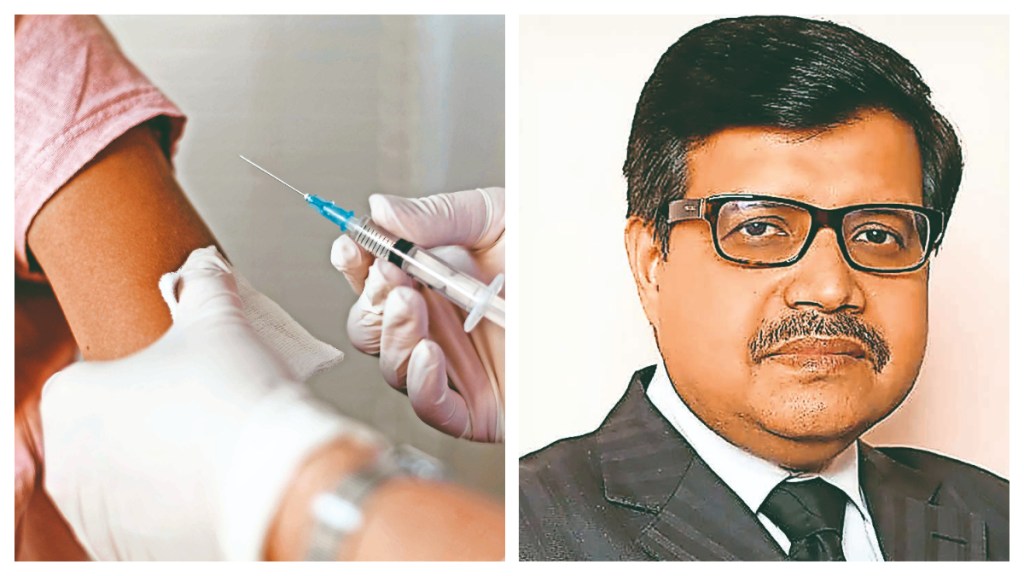
A new study reveals herd immunity for Human Papilloma Virus (HPV), indicating protection even for those unvaccinated. Does this mean the vaccine is proving to be inefficient or unnecessary? Dr Suranjit Chatterjee, senior consultant, internal medicine, Indraprastha Apollo Hospitals, says: “No, herd immunity actually shows the vaccine is highly effective-not inefficient. Herd immunity occurs when a large portion of the population is vaccinated, reducing the virus’s circulation and indirectly protecting even those who are unvaccinated.
This doesn’t mean vaccination is unnecessary; rather, it highlights how well the vaccine works in preventing HPV transmission. However, herd immunity may not be uniform across all regions or HPV strains, and unvaccinated individuals remain at some risk. Continued vaccination is crucial to sustain this protective shield, especially as new generations grow up and vaccine coverage varies. Without ongoing immunisation, herd immunity can weaken, allowing the virus to resurface.”
Is the domestically produced HPV vaccine also showing similar results, or likely to after years of use?
India’s domestically produced HPV vaccine, Cervavac, is relatively new but expected to show similar outcomes over time. It targets high-risk HPV strains (mainly 16 and 18), responsible for most cervical cancers, just like imported vaccines. Early studies and immunogenicity data indicate strong immune response and comparable efficacy. However, herd immunity builds only when large-scale, long-term vaccination programmes achieve high coverage, especially among pre-adolescent girls and boys. Countries using HPV vaccines for over a decade have seen sharp declines in HPV infections and precancerous lesions. India’s similar results will likely emerge after widespread adoption and sustained public health efforts. Thus, while immediate herd immunity data may not yet exist for Cervavac, projections and early findings are promising.
Do you still recommend the vaccine for youngsters?
Yes, vaccination is strongly recommended for youngsters. The HPV vaccine works best before exposure to the virus-ideally before sexual activity begins-making preteens the primary target group. Getting vaccinated early ensures strong immune protection and drastically lowers the risk of cervical, anal, throat, and other HPV-related cancers later in life. Even in the era of herd immunity, direct vaccination provides personal, lifelong protection, regardless of broader community coverage. Relying solely on herd immunity is risky because it can vary between regions or weaken over time. Vaccinating both boys and girls ensures a more complete break in HPV transmission and equitable cancer prevention. Hence, for maximum protection, both national and global health agencies continue to recommend routine HPV vaccination for all eligible adolescents.
Till what age can the vaccine be given, and why is it important for males too?
The HPV vaccine is ideally given between ages 9 and 14, but it can be administered up to age 26. In some cases, adults aged 27-45 may also receive it after consulting a doctor, though the benefits reduce with age due to possible prior HPV exposure.
Vaccinating males is equally important because HPV can cause penile, anal, and throat cancers, and men play a key role in transmitting the virus to partners. Immunising boys not only protects their health but also strengthens community-wide prevention by curbing HPV spread. In short, vaccinating both sexes helps achieve broader herd immunity and ensures gender-inclusive protection against HPV-related diseases.