Mpox Outbreak: Mpox, a highly infectious zoonotic disease, has now become a global threat. Last week, the World Health Organization (WHO) declared the mpox outbreak as a public health emergency of international concern.
“The emergence of a new clade of mpox, its rapid spread in eastern DRC, and the reporting of cases in several neighbouring countries are very worrying. On top of outbreaks of other mpox clades in DRC and other countries in Africa, it’s clear that a coordinated international response is needed to stop these outbreaks and save lives,” Dr. Tedros said in a statement.
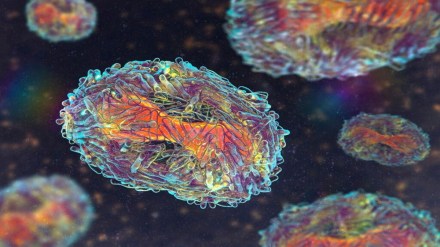
This PHEIC determination is the second in two years relating to mpox. Caused by an Orthopoxvirus, mpox was first detected in humans in 1970, in the DRC. The disease is considered endemic to countries in central and west Africa.
In 2024, cases of mpox linked to MPXV clade Ia have been reported in the Central African Republic and the Republic of Congo, and cases linked to MPXV clade II have been reported in Cameroon, Côte d’Ivoire, Liberia, Nigeria and South Africa.
How Mpox virus spreads?
Mpox, formerly known as Monkeypox, is an infectious viral disease that can spread between people, mainly through close contact, and occasionally from the environment to people via objects and surfaces that have been touched by a person with mpox.
Endemic in central and West Africa, the infectious disease later caused a global outbreak in 2022, leading to a WHO public health emergency in July as it became a multi-country outbreak.
What are the symptoms of Mpox?
Common symptoms of Mpox includes:
- rashes,
- fever,
- headache,
- muscle aches,
- back pain,
- low energy and
- swollen lymph nodes.
“The rash looks like blisters and can affect the face, palms of the hands, soles of the feet, groin, genital and/or anal regions, mouth, throat or the eyes. The number of sores can range from one to several thousand,” the United Nations said in a statement.
It also stated that people with mpox are considered infectious at least until all their blisters have crusted over, the scabs have fallen off and a new layer of skin has formed underneath, and all lesions on the eyes and in the body have healed. Typically this takes two to four weeks. Reports show that people can be re-infected after they’ve had mpox.
Moreover, people with severe mpox may require hospitalisation, supportive care and antiviral medicines to reduce the severity of lesions and shorten time to recovery.
Who is at risk?
In most cases, the symptoms of mpox go away on their own within a few weeks with supportive care, such as medication for pain or fever, but, in some people, the illness can be severe or lead to complications and eventual death.
According to the United Nations, newborn babies, children, people who are pregnant and people with underlying immune deficiencies – such as from advanced HIV – may be at higher risk of more serious mpox disease and death.
“Mpox primarily spreads through close physical contact with an infected person, including skin-to-skin contact, contact with body fluids, and respiratory droplets. Household members of individuals infected with mpox and healthcare workers are at a higher risk of catching the infection,” Dr Tushar Tayal, Consultant, Internal Medicine, CK Birla Hospital, Gurugram told Financial Express.com.
Dr. Tayal also said that mpox has also been reported to spread through sexual contact.
“For People living in or traveling to areas where mpox outbreaks are occurring , they are at increased risk of catching the infection. People with weakened immune systems, including those with HIV, people with chronic illnesses like diabetes and heart disease may be at higher risk of severe mpox if they become infected,” he emphasised.